 Physical therapy and occupational therapy coding and billing can be quite challenging. As is the case with most specialties, providers need to be aware of what’s expected by each payer to ensure proper reimbursement.
Physical therapy and occupational therapy coding and billing can be quite challenging. As is the case with most specialties, providers need to be aware of what’s expected by each payer to ensure proper reimbursement.
Here are six tips to help you avoid physical therapy denials. These tips will ensure proper coding to avoid payer scrutiny, and make sure your practice remains on track towards appropriate reimbursement.
1. Document the Complexity of Therapy Evaluations
The new CPT codes, announced in January 2017, specify three levels of complexity; low, moderate and high. It’s critical that therapists understand and document the specific elements that support these levels.
The CPT Manual serves as a great resource. The included descriptions for these new codes include all relevant documentation components that should be considered when documenting. Refer to codes 97161-97163 for PT evaluations and codes 97165-97167 for OT evaluations for additional information.
Therapists must be selective and accurate with their coding to avoid physical therapy denials. As an example, when using CPT code 97167 (OT evaluation, high complexity), the documentation must support an assessment of five or more deficits that limit the patient’s activities. Complex clinical decision making must also be demonstrated. If these components are not reflected in the documentation, an audit or denial may occur.
Consider the following questions when documenting PT and OT evaluation complexity:
- Did an examination occur? Did it include standardized tests or measurements? These are really the essential points of these codes; going beyond subjective information and including measurable information about the patient’s pain and functional limitations.
- On what criteria is the complexity of the evaluation based?
- What are the treatment options, and how will these treatments benefit the patient?
- Does the evaluation include a clear plan of care with specific goals, frequency, and duration?
2. Specificity Regarding Regions of the Body
Make certain to document the specific muscles and/or joints on which treatment is performed. This helps to justify CPT codes that may require therapy on multiple areas of the body, and helps payers understand specific injuries.
3. Accuracy with Units of Time
The first thing to determine is whether the payer requires all time-based services to be lumped together such as with the Medicare Rule or if each time-based code needs to be listed separately such as with the commercial or AMA Rule. Without identifying what the payer expects, you’re going to have problems getting paid correctly for your services.
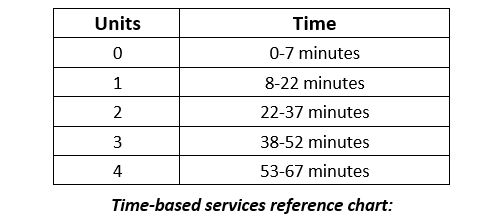
The CPT Manual states that a unit of time is obtained when the provider reaches the midpoint. For PT and OT codes, the midpoint is eight minutes or half of fifteen minutes. This is commonly referred to as the eight-minute rule.
As an example, if a therapist provides five minutes of manual therapy, five minutes of therapeutic exercise, and five minutes of a therapeutic activity following the commercial rule, they would not be able to bill for any of these services because they did not pass the midpoint for any of the services rendered. However, if following the Medicare Rule, the provider could add these services together and bill for one unit of fifteen minutes.
 4. When to use Modifier 59
4. When to use Modifier 59
Modifier 59, which indicates a distinct procedural service, may apply to PT/OT when the same provider performs two timed procedures in two distinctly different blocks of time on the same day. As an example, manual therapy for a patient between 10:15-10:30 and therapeutic exercise between 10:30-10:45. In this case, the provider can bill both services using modifier 59. Add the modifier to the code for therapeutic exercise.
Providers shouldn’t bill time-based codes for more than one patient at a time unless they can show that the services were rendered at completely different times or if a PT or OT assistant (not a technician) assisted with the delivery of care.
One exception is procedures performed in a group setting. For group therapy, bill code 97150 for each member of the group. This is not a time-based code, and reimbursement is typically lower for this service.
5. Timed and Untimed Electrical Stimulation
Therapists should bill CPT code 97032 for attended or timed electrical stimulation, and 97014 for unattended or untimed electrical stimulation. If a therapist is not physically present, with direct contact to the patient, they will not be able to bill for the attended or time-based code. Payers will deny or down-code to the unattended or untimed CPT code. It’s also a good idea to check with your carrier before billing these codes. For instance, Medicare requires the G0283 CPT code for unattended electrical stimulation.
6. Carefully Review the Referral and Utilization Before Rendering Treatment
Does the patient’s current diagnosis match the diagnosis for which PT or OT has been ordered? If it does not, the diagnosis should be clarified prior to treatment being rendered. As an example, this can happen when a patient presents to the ER with pain in one area, receives an order for treatment of that pain but then reports to therapy after the pain has radiated to a different area.
Make certain that the plan of care is medically necessary for the diagnosis and the findings uncovered during the examination. Avoid prolonged, unwarranted treatments to simply increase revenue.
Although not an exhaustive list, these tips can help to improve accuracy and compliance with your PT and OT coding and billing, and avoid physical therapy denials. There’s a lot to consider and implement, but it’s time and effort well invested to ensure fair compensation for services rendered as well as to avoid denials and possible audits.
Read more about our billing services or contact us for information on how we can help your practice with these as well as other issues impacting your revenue cycle.

Nice to read. So useful and informative tips. Many thanks for sharing them all.