 Regardless if you agree with government regulation of healthcare or not, MACRA (Medicare Access and CHIP Reauthorization Act) is here, and it isn’t going away. MACRA will impact small practices in a big way. MACRA is going to have a larger, long-term impact on the healthcare business as we know it. The program starts in 2017 with the first penalties and incentives being paid in 2019.
Regardless if you agree with government regulation of healthcare or not, MACRA (Medicare Access and CHIP Reauthorization Act) is here, and it isn’t going away. MACRA will impact small practices in a big way. MACRA is going to have a larger, long-term impact on the healthcare business as we know it. The program starts in 2017 with the first penalties and incentives being paid in 2019.
What is MACRA?
MACRA is CMS’ newest legislation to move healthcare to a value based system. It’s a system that rewards providers for providing low cost and effective healthcare to their patients. On the other hand, low performers are penalized in the form of decreased reimbursements from Medicare. CMS has already achieved their first goal of having 30% of Medicare payments tied to quality or value through alternative payment models. Their next goal is to increase it to 50% by the end of 2018. MACRA is the method in which they will achieve this goal.
MACRA is basically broken down into two quality programs: MIPS (Merit-based Incentive Payment System) and APMs (Alternative Payment Models). Most providers will be subject to MIPS. The PQRS, Value-Based Modifier, and Meaningful Use programs have all been rolled into MIPS.
Commercial payers are keeping a close eye on MACRA, and many are looking at goals similar to what CMS is doing. CMS is even looking at methods to reward providers who are participating in similar value-based programs from commercial payers.
It’s Too Complicated!
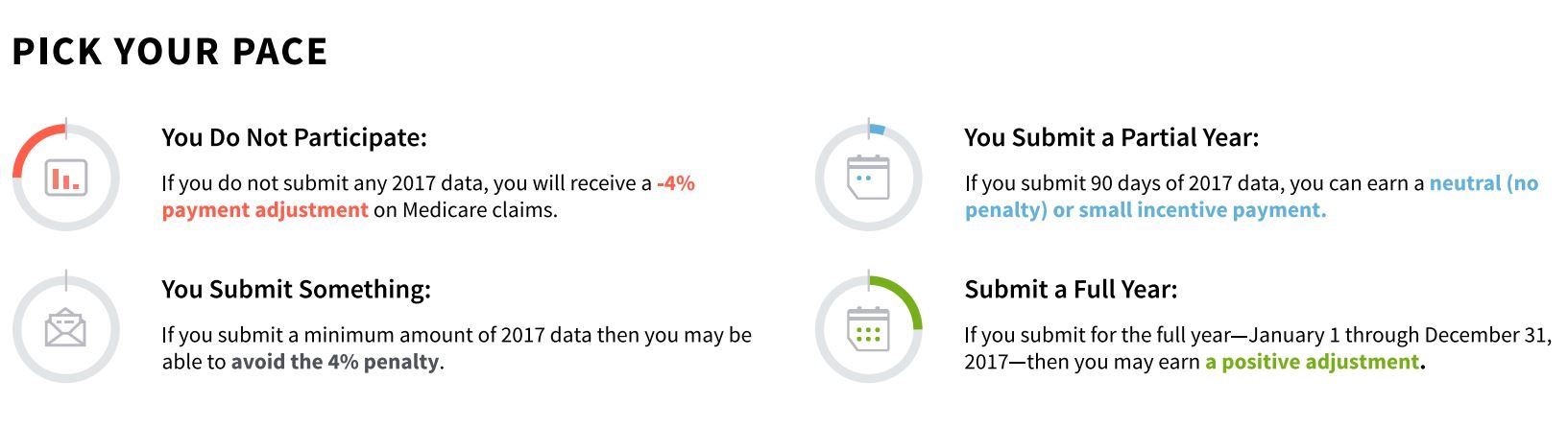
Unlike previous programs, CMS has really tried to simplify and consolidate things. Providers can still avoid a penalty by submitting something in 2017. Obviously, submitting a full year’s worth of data will increase your chances of earning a positive adjustment. Submit nothing at all, and you will receive a -4% payment adjustment on Medicare claims.
If you will be participating in MIPS, your first performance period begins in 2017 to avoid penalties in 2019.
If a provider is already participating in PQRS, Meaningful Use, and the Value-Based Modifier, navigating through MACRA and having a successful submission shouldn’t be too difficult.
Keys To Success
- Get familiar with the Quality Payment Program now
- Make sure you’re using a 2014 or later certified EHR
- Estimate your MIPS score
- Look for opportunities to implement clinical practice improvements
- Identify deadlines and timetables
- Stay up to date with any changes or requirements
- Provide high quality care to your patients
We have partnered with the industry leader in successful PQRS and MIPS submissions, Mingle Analytics. As a leading CMS-Qualified Registry, Mingle has made successful submissions on behalf of over 32,000 providers with a success rate greater than 99%. Choosing Advanced Medical Billing and Mingle Analytics as your submission partners is the best way to ensure maximum reimbursement from Medicare and to avoid costly penalties that can negatively impact your practice.
Visit our MIPS page for more details on how we can help your practice. You can also contact us now for more details.

Leave a Reply